Approximately 1.25 million American children and adults have Type 1 Diabetes (T1D) as a consequence of the individual’s immune system destroying the insulin-producing beta cells (islet) in the pancreas. Adolescents with Type 1 Diabetes do not have a normal number and function of Foxp3+ regulatory T cells (Tregs), a type of white blood cell that is a critical immune regulator to maintaining tolerance and limiting autoimmunity. A major challenge for treatment of T1D is to identify treatments that reset the immune response, and result in long-term beta cell preservation.
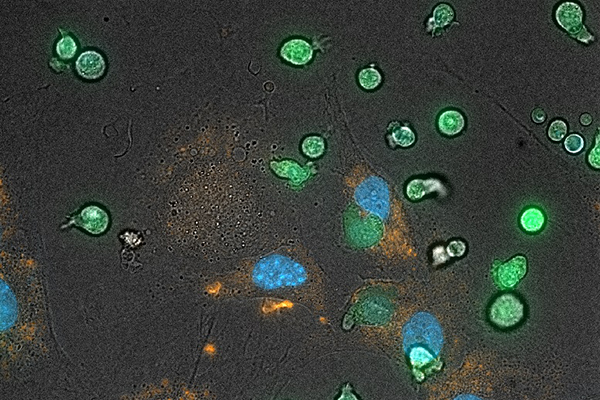
Tregs play a crucial role in maintaining control of an individual’s immune system through their inhibition of T cells that in the setting of Type I Diabetes attack islet cells abnormally. Cleveland Cord Blood Center researchers are studying T cells from normal newborn babies’ umbilical cord blood which are unique in their very strong T regulatory capacity that is related to immune tolerance between the baby and the mother during pregnancy. The CCBC researchers are applying the cell biology knowledge gained in investigating neonatal immune tolerance to the understanding of a baby’s Tregs to treat patients with Type 1 Diabetes.
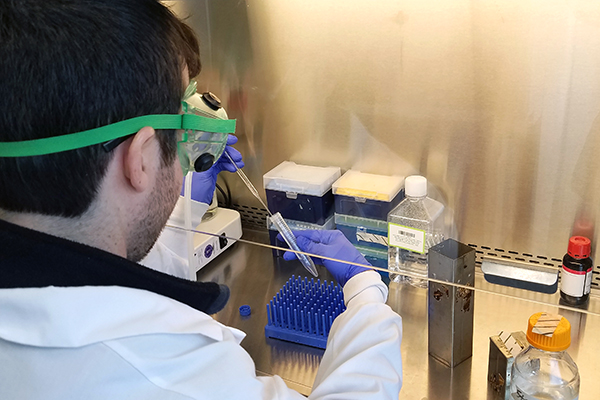
The CCBC researchers expect the Tregs to safely suppress the ongoing abnormal T cell attack on the patient’s islet cells in the pancreas allowing beta cell recovery, and improvement or resolution of the disease. If our current pre-clinical studies support our consideration that Tregs from umbilical cord blood (UCB) can suppress abnormal T cell immune activity against beta cells in the pancreas and re-establish normal insulin/glucagon production, the treatment approach we envision would include isolating CD4+ T cells from a UCB unit that is HLA matched to the patient, generate inducible Tregs (iTregs) and grow these cells for three weeks in sterile culture conditions uniquely developed by our team to maintain T regulatory function. These expanded UCB Tregs would then be infused into the patient with T1D.
The goal is that our UCB iTregs are more potent in their suppressive function to control abnormal activated T cells, and this suppressive function is better maintained over time for cell therapy.
In addition to applications in T1D, the CCBC Research team is concurrently investigating the use of Tregs as a possible treatment of Graft vs Host Disease (GvHD) and diabetic retinopathy.
Published research: Foxp3 expression in induced T regulatory cells derived from human umbilical cord blood vs. adult peripheral blood; Received: 26 January 2018 / Revised: 9 April 2018 / Accepted: 11 April 2018 / Published online: 9 May 2018 / © Macmillan Publishers Limited, part of Springer Nature 2018