While tied to a variety of causes, chronic infection is the main barrier to wound healing. A significant percentage of infected, chronic wounds are tied to complications of diabetes and diabetic ulcers. In addition, certain bacteria have been able to resist conventional antibiotics and antimicrobials by either adopting a resistant form called a biofilm or through the emergence of new, antibiotic-resistant strains.
Despite standard clinical treatment such as wound dressing and debridement of necrotic tissue, wound infection can lead to limb amputation, with patients facing a five-year survival rate of 27 percent.
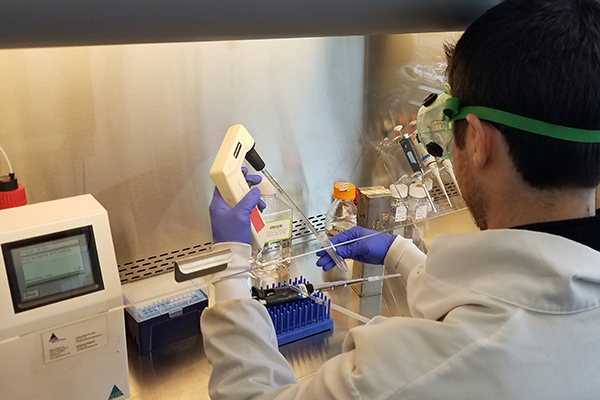
The Cleveland Cord Blood Center’s (CCBC’s) Wound Healing Project has launched into its next phase of exploration. The research team is investigating how umbilical cord blood monocytes and platelet rich plasma may prove helpful in treating patients with chronic infected wounds who are at greatest risk of amputation. These patients often include diabetics, burn victims, and those with pressure ulcers.
Monocytes from umbilical cord blood provide a rich source of cellular and secreted factors for injury and chronic wounds. The high concentration of these factors may explain why infants heal wounds without scarring, unlike adults.
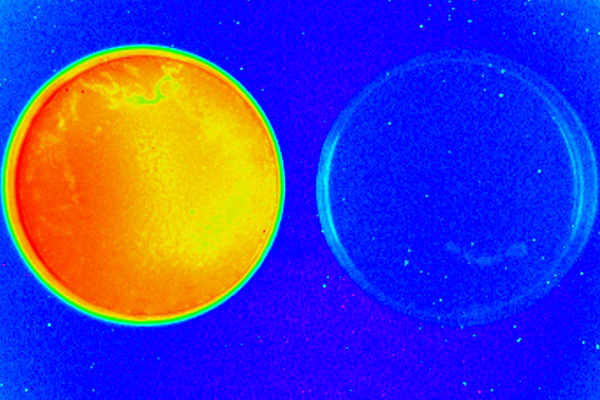
We are focusing on two problems – combating multi-drug resistant forms of bacteria such as Pseudomonas aeruginosa, and penetrating the biofilm surrounding and protecting the bacteria, both of which make successful treatment with conventional antibiotics highly challenging.
We are collaborating with biomaterials experts at the University of Illinois Chicago to determine an effective therapeutic cell scaffold material to use to hold the therapy at the site of infection. These products are currently under development towards regulatory approval.
Animal testing has been launched using a mouse model for proof of concept and safety. The research is being conducted in partnership with the Case Western Reserve University Institutional Animal Care and Use Committee. Preliminary results are anticipated for later in 2022. We have a good amount of evidence that our approach penetrates bacterial biofilms, while most antibiotics do not. We’re looking to show that bacterial biofilm penetration by our therapeutic results in the clearance of infected wounds in a mouse model.